Smarter Mental Health
Cut Behavioral-Health Claims Up to 20% with Preventive AI Care
Brightn gives members always-on mental-wellness support, lowering high-cost interventions and differentiating your plan in a crowded market.
93%
In-App User Satisfaction Rate
3x
Better than industry average 30-day retention rates
30 days
To measurable change

.png)










































brightn
Chosen by Plans That Bet on Outcomes
Brightn empowers health plans to support the full spectrum of wellbeing — health, wealth, and purpose — for lasting behavioral change.
"I think that's also one of the things that's challenging. As we explored the partnership — and even just the product that Brightn provides — we realized that health is one component of wellbeing. But wealth and purpose are two other equally weighted components of wellbeing and of brain health”


.png)
The Claim Cost Surge You Can’t Ignore
Rising behavioral-health costs are putting pressure on payers to find partners who can deliver measurable ROI.

20% annual growth in behavioral-health claims is compounding costs year over year.

7 in 10 employees report at least one mental-health symptom.

84% of those affected say workplace factors are a root cause.

0 interest in point solutions—self-funded groups want real ROI.
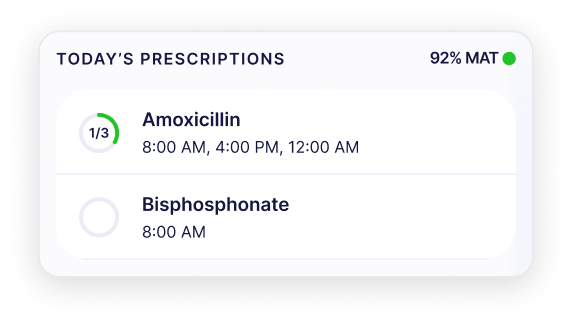
Brightn in Action
Precision Tools, Immediate Impact
Risk-stratified coaching, MedOne-validated adherence nudges, and population-level analytics intercept high-cost episodes before they ever hit your loss sheet.
Risk-stratified coaching & prompts
Reduces severe episodes that trigger costly inpatient care
.png)
Medication-adherence nudges
Improves outcomes, lowers readmissions
.png)
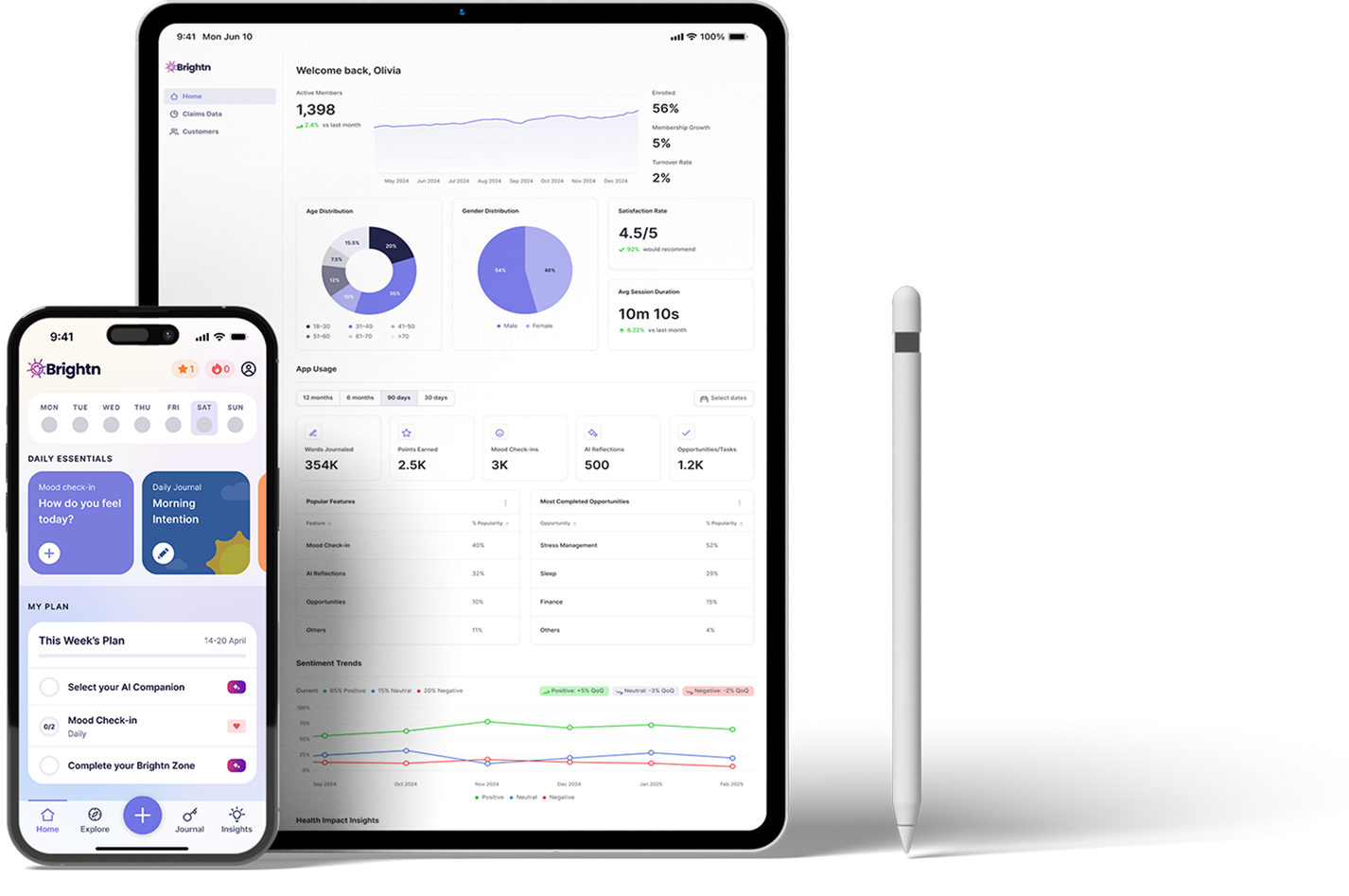
Population analytics dashboard
Pinpoints high-risk cohorts for targeted programs
.png)
Performance Metrics
Metrics That Move
Your MLR
Your MLR
93% of users report high in-app satisfaction — after just 30 days.
Early intervention cuts downstream costs tied to ER visits and specialty therapy.

93%

In-App Satisfaction after 30 Days

See your projected PMPM savings
Get a personalized breakdown of your potential PMPM savings based on your member population.

Frequently Asked Questions
for Health Plans
for Health Plans
How does Brightn help reduce behavioral-health claims?
High-risk individuals are flagged early through behavior patterns, allowing care teams to intervene proactively. Brightn also improves prescription adherence by helping members stay emotionally regulated and engaged in their care plan. Brightn prevents issues from escalating by supporting members before they reach a breaking point. With daily journaling, mood tracking, and personalized content, members develop healthier coping habits and reduce reliance on high-cost interventions.
Is this a replacement for clinical care or an EAP?
No—it’s a complement. Brightn fills the “pre-clinical” gap where 70%+ of distress lives. We increase upstream engagement, which boosts downstream adherence and reduces overreliance on crisis care. Brightn is also included in EAPs, giving members support between sessions and improving overall outcomes.
How do you prove ROI?
We provide detailed utilization reports, engagement metrics, and aggregate mental wellness outcomes. Plans using Brightn with pharmacy claims oversight (e.g., MedOne) have seen medication adherence improve and care costs drop.
What’s the implementation lift?
Minimal. We provide a turnkey onboarding process, digital collateral, and hands-on support. Your members get instant access via email, text, or benefits portal integration.
Can this help us satisfy mental-health parity or value-based care goals?
Yes—Brightn supports parity by improving access, engagement, and measurable outcomes. It fits seamlessly into value-based frameworks and supports risk-based contracts through preventive mental wellness support.









